Blog posts
The role of economic evaluation in the CAREPATH project
Published on 5 May 2022The economic evaluation (EE) of healthcare technologies has become in many European countries and worldwide a basic tool for reimbursement, pricing and purchasing decisions
Public decision makers have the difficult task of combining a double objective: on the one hand, they should identify and favor access of citizens to those therapeutic advances that bring additional health benefits; on the other hand, they should prioritize and implement those interventions, strategies and policies with acceptable value for money under increasingly tight public budget constraints in order to guarantee the financial sustainability of public health systems. In this context, the EE is a tool of undoubted utility when it comes to establishing an explicit and comprehensive framework where health and social costs are compared with therapeutic and social benefits and considered in the decision process in order to improve value for money.
What does an economic evaluation consist of and what objectives does it pursue?
The economic evaluation is based on the need to consider not only the efficacy and security of health interventions and/or technologies for decision-making, but also the resources used in the process. From an economic perspective, the most relevant concept of cost is the so-called opportunity cost.
The opportunity cost of a health intervention can be interpreted as the monetary valuation of said resources. However, the opportunity cost also represents the loss of health and well-being benefits that would have been reached if the resources were used in the best alternative. The synonym of opportunity cost is, therefore, sacrifice.
In this way, the economic evaluation should be interpreted as one more link in the evaluative chain
EE is defined by Drummond et al. as a comparative analysis of alternative courses of action in terms of both their costs and consequences
Since it involves some kind of comparison between alternative treatments, programs and interventions, the correct way to compare two alternatives is to assess what additional costs and effects which are incurred or obtained from a given intervention versus its best alternative (for instance, the routine clinical practice).
Typically, the most commonly used indicator in EE is the incremental cost-effectiveness ratio (ICER):
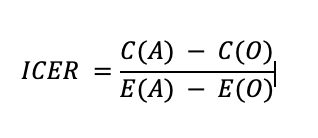
where A is the alternative of interest and O is the current therapy. In the numerator we compare the costs and in the denominator the effects of the interventions. The interpretation of the numerical results of the ratio would indicate the incremental cost of obtaining an additional gain in terms of health.
The relevance of the perspective chosen
The perspective of the analysis is a key element of the evaluation, which can condition the results achieved and the conclusions derived from them. In Alzheimer's disease, health care resources are only part of the resources mobilized to care for people with this disease. There is a series of long-term care, of a non-health nature, provided from the professional field (telecare, day centers, home support services, facilities,...).
Likewise, the main source of support falls on the families. In the literature it is called family care or informal care
Likewise, it is possible to study the effect of an intervention not only on the patient's health but also on the health and well-being of caregivers (known as spillover effects )
A recent work found that in economic evaluations carried out in the field of Alzheimer’s disease interventions “the inclusion of social cost can also influence the results, as 37% of the economic evaluations included became the dominant strategy after including social costs when they were already cost-effective in the health care perspective.”
The role of economic evaluation in the CAREPATH project
The main purpose of the health economic assessment in CAREPATH project will be (i) to estimate the incremental costs (from the societal and National Health System perspective) of the intervention (CAREPATH-an integrated patient-centred approach- in multimorbid elderly patients with dementia) vs. control, (ii) to reveal the incremental cost per unit of benefit of switching from usual care to the CAREPATH approach, and (iii) to determine whether the CAREPATH approach is a cost-effective option. Therefore, the EE would reveal whether or not the CAREPATH intervention entails not only an improvement in terms of health/clinical outcomes but also in terms of costs. In other words, we will test if CAREPATH is a cost-saving alternative or a “good value for money” intervention in comparison with the usual care in such a target population.
The literature available (FamTechCare , LIVE@Home.Path , D-CARE, Namaste Care Family program , BeyondSilos , TV-AssistDem, PARO) regarding EE of health interventions for the management of conditions of elderly multimorbid patients with dementia is scarce. In addition, a great heterogeneity is observed between the interventions both in their design, which are usually multicomponent, focused both on the care of the person with dementia and their caregiver, and in their assessment, with different outcome measures and target population with different severity of dementia. All this makes it difficult to compare existing interventions.
Conclusion
Health interventions with multiple components represent a major challenge in the field of evaluation. One of the pieces of information to integrate in the evaluation of these technologies is the economic one. In this way, our aim is to generate relevant information for decision-making in the dimension of efficient use of available resources.
 This project has received funding from the European Union’s
Horizon 2020 research and innovation programme under grant
agreement No 945169
This project has received funding from the European Union’s
Horizon 2020 research and innovation programme under grant
agreement No 945169